Blood Parasite Smear Test Explained (With Photos)
Detecting many blood parasites, including malaria, depends on the blood parasite peripheral smear test—a simple yet powerful diagnostic tool. This guide demystifies the test, highlighting its use in accurately diagnosing parasitic infections and what to anticipate from the results.
Key Takeaways
Blood parasite smear tests, essential for diagnosing diseases like malaria and filariasis, often aided by Giemsa stain for visual clarity of parasites.
Proper specimen collection, prompt preparation of blood smears, and comprehensive patient travel history are fundamental for accurate test results, reducing the risk of misdiagnosis and ineffective treatment.
Rapid diagnosis with blood parasite smear tests involves a systematic process, utilizing various laboratory techniques and technologies
Understanding Blood Parasite Smear Tests
The blood parasite smear test is diagnostic tool used to screen for and detect different types of blood parasites, including:
Plasmodium (malaria) species
Trypanosoma (sleeping sickness)
Spirochetes
Babesia (associated with Lyme disease)
Filariasis
These ova and parasite blood tests are incredibly useful in diagnosing diseases like malaria and parasitic infestations. They can even help quantify the level of parasitic infection in the blood, a critical detail when it comes to treatment.
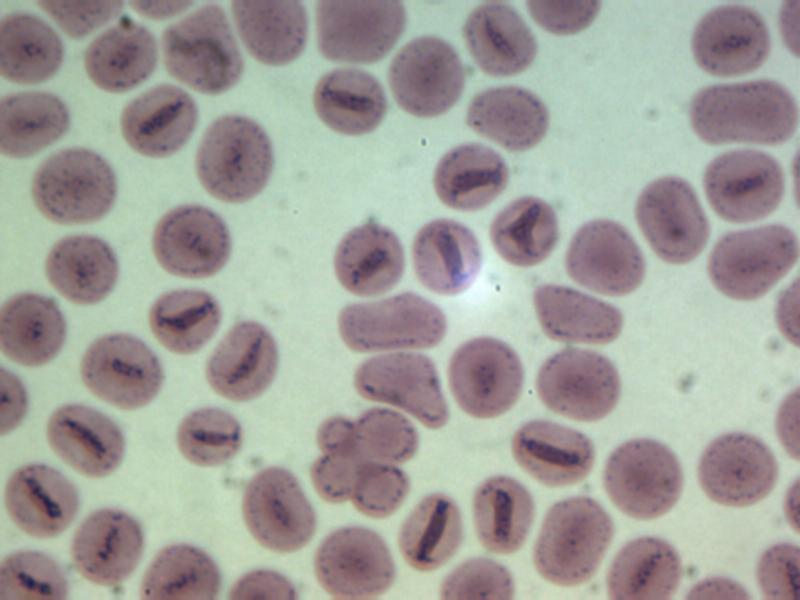
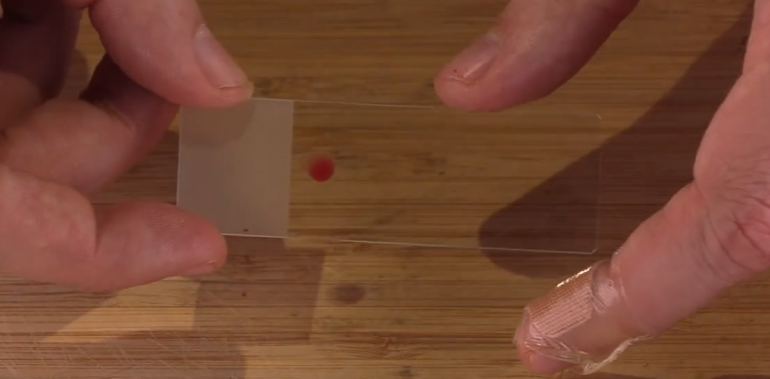
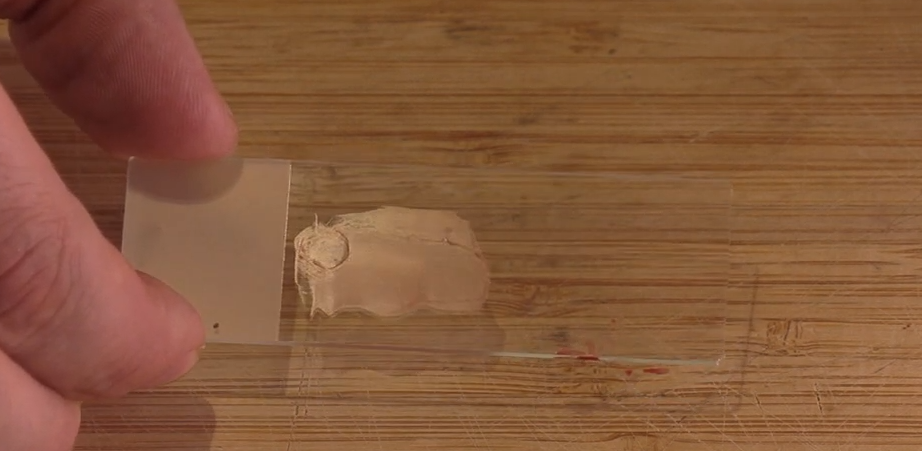
The process of a blood parasite smear test includes checking a thin smear from a blood sample for any parasites. See images below that shows me collecting my blood samples to make a thin film blood smear.

Thick Smears Versus Thin Smears
The detection of blood parasites can rely on the distinct roles of thick and thin smears. A thick blood smear is created by spreading a drop of blood on a glass slide, producing a concentrated layer of blood cells. This method is excellent for screening and picking up even low levels of parasites in the blood.
On the other hand, a thin blood smear involves spreading a drop of blood across a larger area of the slide. The result is a detailed view of individual cells, which aids in the identification of blood parasites.
The main difference between thick and thin smears is that thick smears have more concentrated layers of lysed red blood cells, making parasites more visible, while thin smears allow for a more detailed examination of the parasites’ morphology.
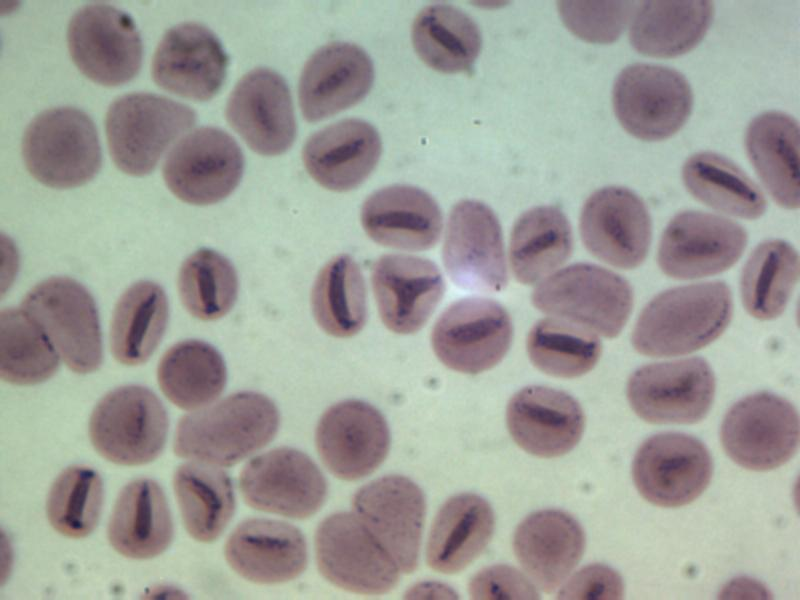
Giemsa Stain: The Key to Visualizing Parasites
In blood parasite smear tests, Giemsa stain serves as a crucial tool. It’s like a color-coding system that makes parasites visible under the microscope. By coloring the blood films, Giemsa stain helps to clearly distinguish the shape of parasites such as ring, rod, and ameboid forms.
This method allows for the easier detection and quantification of various blood parasites, including the malaria parasite and different species of malaria parasites, making it possible to quantify malaria parasites effectively.
The Importance of Specimen Collection

Proper specimen collection is critical for the accuracy of test results. It’s like gathering evidence at a crime scene – every detail matters, and any misstep can impact the validity of the findings.
When collecting blood for parasite smear tests, there is no significant difference between venous blood and blood collected from a pin prick on your finger. It’s important to note that the blood smears should be prepared as soon as possible after collection. This timely preparation aids in making the diagnosis more accurate and quick for patients.
In our thin film blood test, the patient prepares their own blood smears as soon as the blood comes out. This ensures fresh and accurate samples. If something goes wrong, we can just ship a new test kit to them.
Patient Preparation and Travel History
A comprehensive travel and symptom history are integral parts of the specimen collection process. The preparation ensures that the whole blood sample can be used to create blood smears promptly after collection, preventing any changes in the sample that could interfere with the quality of the smears and the interpretation of the results.
Travel history, on the other hand, provides insights into potential exposure to specific parasites. For instance, a recent visit to a malaria-prone region would warrant a specific test for malaria parasites. Healthcare providers typically ask about:
the countries visited
recent travel dates and locations
specific activities during the trip
visits to tropical regions
any history of travel-related illnesses
Identifying Malaria and Other Blood Parasites
Blood parasite smear tests may reliably identify malaria and other blood parasites.
The usual malaria species that show up in blood parasite smear tests are:
Plasmodium falciparum
Plasmodium vivax
Plasmodium malariae
Plasmodium ovale
However, they’re not the only ones. Technicians also need to be on the lookout for other blood parasites such as filariasis, Babesia and other parasitic infections or metabolic issues.
Laboratory Techniques in Detecting Parasites

The laboratory is the heart of the entire process. It’s where blood samples are transformed into insightful data, helping healthcare professionals make informed decisions about treatment plans.
Microscopy plays a significant role in this process, and several techniques are employed to examine thick and thin blood smears. Fluorescent microscopy and the quantification of parasite loads in samples are some of the modern techniques used in labs today.
Microscopic Examination: A Detailed Approach
Examining samples under a microscope is a process that requires precision and attention to detail. It’s like a treasure hunt, with medical professionals looking for the telltale signs of parasites in blood smears.
During the examination, a series of observations are made, including:
The size, shape, and number of blood cells
Any irregularities in blood cells
A differential count
The use of staining techniques to distinguish between different parasite species.
Novel Detection Methods
Advancements in technology have led to the development of new techniques for parasite detection. Deep learning object detection, a modern diagnostic method, uses advanced models to spot and categorize different parasite species in microscope images. This method not only offers enhanced accuracy but could also increases the efficiency of parasite identification.
But obviously these AI techniques are still too immature to be ready for medical testing. We don’t understand the probability of false negatives or false positives…and we know that AI routinely hallucinates things that aren’t real, potentially causing you to seek treatment for a parasite that you may not actually have!
Other newer methodologies like flow cytometry and PCR-based techniques may be employed to identify blood parasites. These techniques further enhance the sensitivity, precision, and reproducibility of the tests. But, PCR techniques are notorious for over-amplifying low amounts of DNA, possibly overreporting the amount of blood parasites present in cases of low infection levels.
Errors and False Negatives of Parasite Blood Smears
Errors in blood parasite smear testing can occur due to a variety of factors, including:
Platelets covering a red blood cell
Overlooking a positive slide
Misinterpreting artifacts as parasites
Mistakes in blood droplet size
Low skill technician analyzing samples.
It’s crucial to use experienced parasitologists to do the analysis. They will be aware of these potential issues and take steps to minimize their impact on test results.
Experienced Parasitologists Ensure More Accurate Test Results
The skill and experience of the technician carrying out the test is paramount. For this reason, we have 2 experienced PhD parasitologists to analyze 100% of our patient’s samples for parasites.
Summary
In conclusion, blood parasite smear tests are a powerful tool in diagnosing malaria and other parasitic infections. From the collection of the blood specimen to the microscopic examination of the smears, every step is critical in ensuring accurate results. While the tests are not without limitations, we’re hoping that advancements in technology and proper specimen handling can significantly enhance their accuracy and reliability.
Frequently Asked Questions
How Long Does It Take To Get Test Results Back?
The timing depends on the laboratory. After the lab receives the sample, it can be 3-4 days. When I took this test at quest lab and Cab Corp, both took about 3-4 days after receipt of the sample. When I took our thin film blood smear test, it took 3 days to get test results back, not including shipping time.
Does the thick or thin film blood test check for all parasites?
No, think/thick film blood tests only check for the parasites that live in the blood, and are visually identifiable in the blood. Intestinal parasites are best identified via a stool test, but there are antibody based blood tests that can test your blood and find evidence of exposure to intestinal parasites.
Which parasite can be detected by the thick blood smear?
The thick blood smear test is used to detect the presence of malaria parasites. If initial tests are negative, repeated blood smears are recommended to confirm the absence of malaria infection. This tests is useful for North Americans, since malaria has almost been exterminated from the USA.
What are the symptoms of a blood parasite?
The symptoms of a blood parasite may include fever, depression, weight loss, poor body condition, muscle weakness, discharge from the eyes, and bloody diarrhea. Additionally, some people may experience flu-like symptoms such as fever, chills, sweats, headache, body aches, loss of appetite, nausea, or fatigue. Various blood parasite testing methods can be employed to detect blood parasites.
What is a blood parasite smear test?
A blood parasite smear test is a diagnostic test that can detect various types of blood parasites and blood metabolic issues, making it especially effective in diagnosing malaria and other parasitic infections.
What is the difference between thick and thin smears?
The main difference between thick and thin smears is that thick smears have a concentrated layer of lysed red blood cells, allowing parasites to be more visible, while thin smears offer a more detailed examination of the parasites’ morphology. This can help in making a more accurate diagnosis.
